FieldStrength MRI magazine
User experiences - April 2015
Efficiency and diagnostic confidence drive adoption of three recent imaging techniques in pediatric neuro exams at Phoenix Children’s Hospital
At PCH, fast, high resolution susceptibility weighted imaging with SWIp is now routine for traumatic brain injury imaging. Fast contrast-free perfusion imaging with pCASL is used in all patients with acute cerebrovascular accidents or abnormalities such as acute stroke. The excellent fat suppression of mDIXON TSE has become the standard at PCH for fat suppression in the spine and extremities, for imaging lesions in the soft tissues of face and neck, and for contrast enhancing abnormalities that are mostly visible with fat suppression.

Jeffrey H. Miller, MD, is Pediatric Neuroradiologist and Radiologist Director of MRI at Phoenix Children’s Hospital. His academic affiliations include Clinical Assistant Professor of Radiology, University of Arizona College of Medicine, the Mayo Clinic-Scottsdale and the Barrow Neurological Institute at Phoenix Children’s Hospital. His current research interests are functional MRI, MR connectomics, and brain PET-CT. Dr. Miller has lectured extensively on advanced pediatric MR imaging.
“We rely on the high resolution and robust imaging capabilities of our Ingenia systems.”
Advanced MRI for challenging cases
Phoenix Children’s Hospital (PCH, Phoenix, Arizona, USA) is the primary referral children’s hospital for the state of Arizona, serving patients with the most complicated cases. The hospital is using two Ingenia 3.0T systems and two 1.5T systems. “We’re a referral center for complex diseases affecting neurological systems, especially traumatic brain injury, brain tumors, epilepsy, and vascular diseases including stoke,” says PCH neuroradiologist Jeffrey H. Miller, MD. Along with Lead MRI Technologist Amber Pokorney, Dr. Miller utilizes advanced MRI techniques in some of the hospital’s most challenging imaging cases.

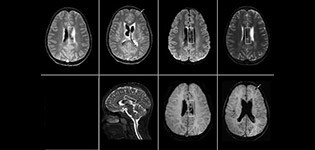
SWIp supports diagnostic confidence in traumatic brain injury
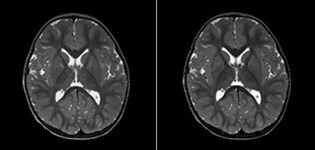
The value of susceptibility weighted imaging in visualizing brain injury is well documented. The Philips multi-echo SWIp technique provides fast susceptibility weighted imaging with enhanced susceptibility contrast and high resolution.
“Pediatric imaging is not without its challenges,” Dr. Miller says. “Since our patients are often very small, we need very high-resolution imaging. In cases of brain injury, we need to obtain information quickly so the treating clinicians can make decisions on care. We rely on high resolution and robust imaging capabilities, and SWIp provides that.”
“SWIp helps us identify blood or blood products, calcification, and diseases that affect the vascular system,” says Dr. Miller. “In children with traumatic brain injuries, it highlights areas that are injured, better than some of the previous techniques that we were using. These children often have micro-injuries that cause small amounts of blood or tissue damage. Adding SWIp helps us to better characterize the extent and nature of the injury. Having characterized an injury to the extent of what’s possible supports our diagnostic confidence.”
Full adoption after initial comparison
“I would definitely recommend other users to implement SWIp. We initially added the SWIp sequence following a lot of support for its utility in the literature. Then we directly compared SWIp to the 2D gradient echo sequences that we were using. After a good amount of clinical experience in seeing its benefits, we were confident to replace the old sequences with SWIp. It gives us a better assessment of the physiological processes of the brain that were less apparent on our previous imaging sequences,” says Dr. Miller. “SWIp is now a routine sequence for imaging traumatic brain injury patients at PCH, and it’s episodically added for patients who have intracranial vascular abnormalities.”
“I believe SWIp is rapidly becoming the standard in imaging traumatic brain injury, because of its high sensitivity to venous blood products. SWIp may even help attract patients; our neurosurgeons often ask to have the patients imaged on our scanners with highly sensitive techniques like SWIp. There’s also a growing application of SWI sequences in other vascular abnormalities because of the possibilities around physiological assessment of the brain than just a standard structural imaging.”
“We use pCASL to help delineate the perfusion abnormality.”
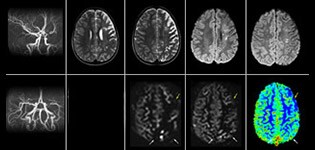
pCASL helps assess brain perfusion without contrast
Pseudo-continuous arterial spin labeling (pCASL) was developed for brain perfusion imaging without contrast agent. “This is very desirable in pediatric patients where the general trend is to limit the administration of contrast,” says Dr. Miller. Growing confidence in specific applications “We built up confidence in pCASL by comparing it to contrast-based perfusion imaging. Once we had confidence that it was representing what the contrast perfusions were representing, we increased our diagnostic confidence by serial imaging in either the acute stage or the long term stages in a number of patients with arterial abnormalities.
Dr. Miller uses pCASL for all patients who present with chronic and acute cerebrovascular abnormalities such as acute stroke, as well as patients who present with signs of acute inflammation in the brain, and occasionally in patients with tumors, to assess the perfusion status of their tumor.
“In combination with diffusion weighted imaging, it can help give a more extended assessment of the degree of perfusion abnormality in a patient who is suffering acute ischemia. We have a number of patients who have chronic arterial insufficiency due to prior arterial abnormalities or acquired arterial abnormalities such as sickle cell disease or neurofibromatosis. Sometimes the child’s first manifestation of disease progression is a reduction in brain perfusion before stroke symptoms manifest clinically or in diffusion weighted imaging. We use pCASL to help delineate the perfusion abnormality.”
To other new users I would recommend to also start to interpret the pCASL images in comparison with other standard imaging – T2 and FLAIR and DWI – until the user gains confidence in interpreting these images by themselves.” “A powerful use of pCASL is in patients with chronic cerebrovascular stenosis, where clinicians desire information on how compensatory mechanisms of the brain are performing to enable perfusion to the brain. Often clinicians take into account how the compensatory mechanisms appear to help to provide adequate perfusion to the patient’s brain, and they may intervene surgically or make some other management decision.” “Another special application is the assessment of cerebrovascular reactivity with a Diamox perfusion exam, where we subtract two sets of pCASL images.”
Efficiencies gained with pCASL
“pCASL has now become more of a first-line scan for assessing perfusion for us, as opposed to DSC-based perfusion imaging with contrast agent. And in patients who were not planned to have contrast, we can perform pCASL for perfusion imaging without need to stop the exam, pull the patient out, and put in an IV. It also negates the postprocessing that’s necessary for dynamic susceptibility contrasts. And it allows us to repeat perfusion imaging in the same patient at the same imaging time, which is helpful in terms of patient motion, or in a situation where a scan needs to be done before pharmacological perfusion imaging.”
“mDIXON TSE has been a significant improvement compared to imaging sequences that we have utilized to date.”
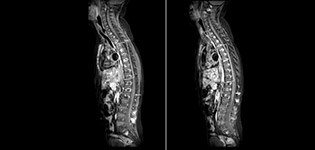
Routinely obtaining homogeneous fat suppression under virtually all conditions with mDIXON TSE
Philips mDIXON TSE is a two-point DIXON technique that separates water and fat signals, for time-efficient fat-free imaging, even in challenging neuro anatomy. “mDIXON TSE has been one of the most significant improvements in imaging sequences that we have utilized to date at PCH,” says Dr. Miller. “Its multi-parametric acquisition allows us to obtain fat suppressed images and equivalent non-fat suppressed T2 images all in the same sequence. In addition, prior methods of fat suppression could be artifactually corrupted by poor patient anatomy or poor operator application, but with mDIXON we now have a robust and reliable method of fat suppression.” Fat saturation is historically challenging at the ends of fields of view, especially in total spine imaging and in difficult patient anatomy such as the lower regions of the neck. “Due to the unique fat suppression capabilities of mDIXON, however, these challenges no long apply,” says Dr. Miller. “We routinely obtain homogeneous fat suppression under virtually all conditions. It has also led to some efficiencies by not having to repeat sequences because of that technical failure.”
mDIXON TSE makes a difference
“mDIXON TSE has increased our diagnostic confidence in ruling in or ruling out abnormalities in which fat suppression is critical to diagnosis, such as metastatic disease or osseous abnormalities.”
“mDIXON TSE is most useful in patients with lesions or abnormalities in the soft tissues such as the face and neck, and for patients with contrast enhancing abnormalities that are mostly visible with fat suppression,” says Dr. Miller. “All our spine imaging now routinely contains mDIXON water-only T2 images, and this allows us to identify pathology that may be obscured by non-fat suppressed imaging such as injuries of the bone. And it’s not necessary to obtain additional standard TSE T2 images because the in-phase mDIXON images are equivalent to standard TSE T2 images.”
More referrals thanks to powerful techniques
Is using these techniques a good way to attract patients and referrals? Absolutely, says Dr. Miller. “Our neurosurgeons ask to have patients examined on the scanners with SWIp capability, so they can be imaged with highly sensitive techniques. We’ve had a number of neurosurgical cases for children with sickle cell disease come to us to have pCASL imaging specifically. And the robust fat suppression of mDIXON TSE is critical to a number of diagnoses, not only in pediatrics but also for adults, and having a reliable method of fat suppression is definitely a benefit to radiologists and clinicians.”
References
Goetti R, O'Gorman R, Khan N, Kellenberger CJ, Scheer I. Arterial spin labelling MRI for assessment of cerebral perfusion in children with moyamoya disease: comparison with dynamic susceptibility contrast MRI. Neuroradiology. 2013 May; 55(5):639-47, Epub 2013 Feb https://www.ncbi.nlm.nih.gov/pubmed/23404242 Miller JH, Pokorney A, Naidu P, Eggers H, Shar M, Perkins T. Improved Fat Suppression and Field Homogeneity of mDixon TSE Total Spine Imaging compared to SPIR Fat Saturation for Post-Contrast T1-weighted Imaging. Proceedings of the Joint Annual Meeting of the ISMRM-ESMRB. Milan, Italy: International Society for Magnetic Resonance in Medicine, 2014.
Results from case studies are not predictive of results in other cases. Results in other cases may vary.
Results obtained by the facility described in this article may not be typical for all facilities.
“We routinely obtain homogeneous fat suppression under virtually all conditions.”